Peptide Therapy for Longevity: How Anti-Aging Peptides Actually Work
Peptide Therapy for Longevity: How Anti-Aging Peptides Actually Work
Walk into any modern longevity clinic or scroll through social media, and you will quickly encounter the phrase “peptide therapy.” It is often framed as the next frontier in anti-aging: injections or troches of short amino-acid chains that promise better sleep, faster recovery, smoother skin, fat loss, and even an extended healthspan.
Like many ideas in longevity medicine, there is a kernel of real science beneath the marketing hype—but also a great deal of speculation, regulatory grey area, and outright misinformation. In this article, we will take a clear-eyed, evidence-informed look at peptide therapy for anti-aging and longevity:
- What peptides actually are
- How they signal in the body
- Which classes of peptides are genuinely promising
- Where the evidence is thin or overhyped
- The realistic role of peptide therapy inside a structured longevity program
This is not medical advice and is not a substitute for an in-person evaluation with a qualified clinician. Rather, it is designed to help you have a more informed, grounded conversation about peptides and healthy aging.
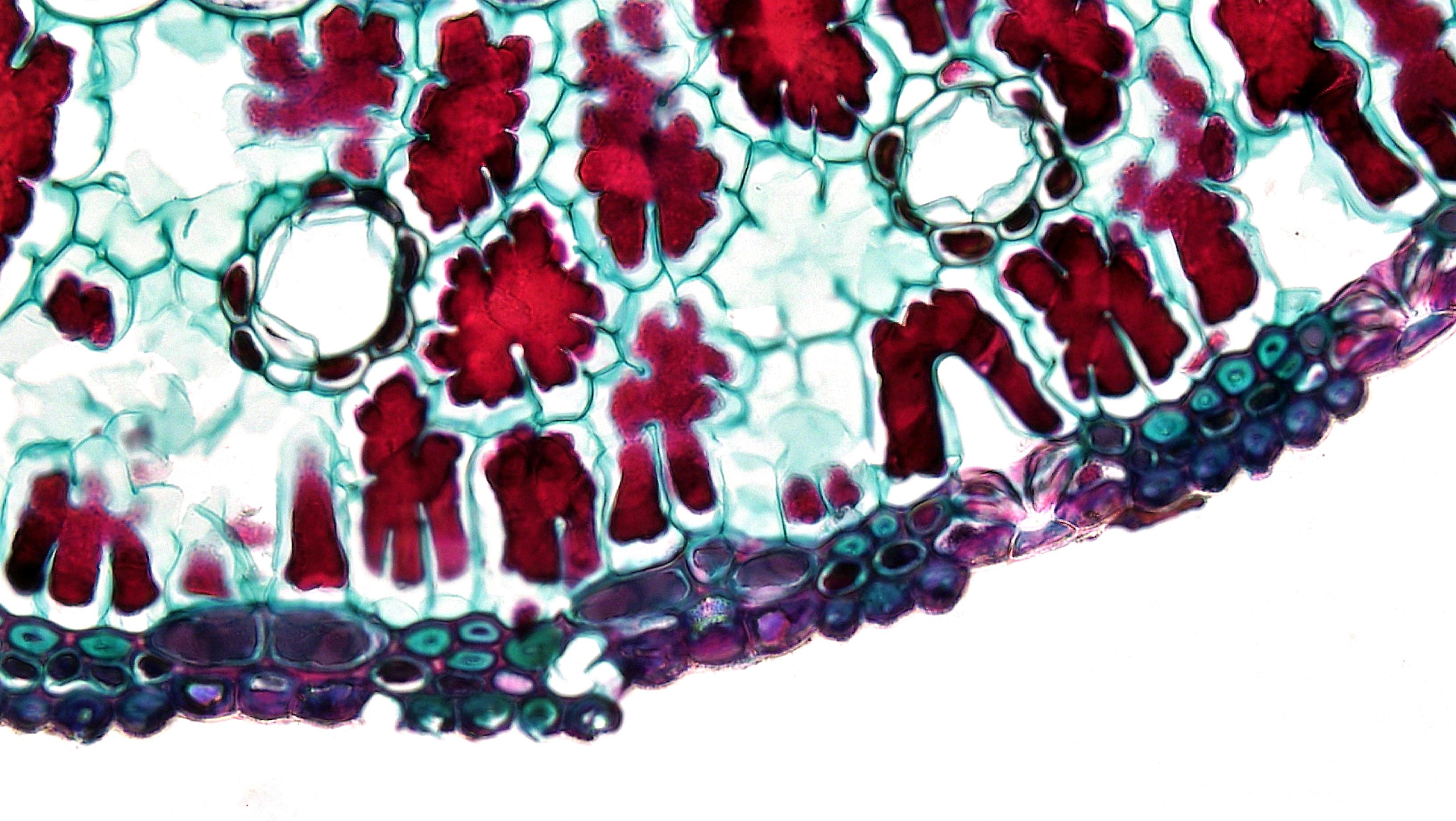
What Are Peptides, Really?
Peptides are short chains of amino acids—typically between 2 and 50—that act as signaling molecules in the body. You can think of them as tiny “instruction notes” that cells use to communicate with one another.
Some well-known examples:
- Insulin is a peptide that directs cells to absorb glucose from the blood.
- GLP‑1 analogs (such as semaglutide) are peptides that influence satiety, blood sugar, and weight.
- Parathyroid hormone analogs are peptides that control calcium and bone metabolism.
These are approved medications with clearly defined indications, doses, and safety profiles.
By contrast, the peptides that dominate anti-aging discussions—such as CJC‑1295, Ipamorelin, BPC‑157, TB‑500, Epitalon, and various “Wolverine stacks”—are not approved by the FDA for longevity or general wellness. Many are sold online as “research chemicals” and compounded by pharmacies in a regulatory grey zone.[^atria]
This distinction matters. The fact that some peptides are FDA-approved medicines does not mean every peptide being sold for “anti-aging” has similar levels of evidence or oversight.
Why Peptides Are So Attractive for Anti-Aging
Peptides sit at the intersection of three trends:
- Molecular precision: We can design peptides to bind specific receptors and pathways, potentially giving more targeted effects than older small-molecule drugs.
- Endogenous biology: Many peptides mimic signals the body already uses—growth hormone–releasing hormones, tissue repair signals, or mitochondrial regulators—making them feel “natural.”
- Rapid commercialization: Because many anti-aging peptides are not formally approved drugs, they can be marketed more quickly through wellness clinics and online vendors.
For people deeply invested in health optimization, this combination is compelling. However, an honest longevity strategy has to separate scientific plausibility from proven benefit.
Core Mechanisms of “Anti-Aging” Peptides
Most peptides discussed in longevity circles fall into a handful of mechanistic buckets. Understanding these categories makes it much easier to evaluate any new peptide you encounter.
1. Growth Hormone Secretagogues
These peptides stimulate the body’s own production of growth hormone (GH) and insulin-like growth factor 1 (IGF‑1). Examples include:
- CJC‑1295 (a growth hormone–releasing hormone analog)
- Ipamorelin (a ghrelin receptor agonist)
- Sermorelin
- Tesamorelin (FDA-approved for HIV-associated lipodystrophy, but sometimes used off-label)
The potential upside:
- Increased lean body mass
- Reduced visceral fat
- Improved sleep architecture
- Better recovery from training
The trade-offs:
From a longevity perspective, the picture is complicated. Many animal studies show that lower GH and IGF‑1 signaling is associated with longer lifespan, not shorter. Some of the longest-lived mouse models and certain human populations with GH signaling defects appear to be protected from age-related diseases.[^atria]
In other words: while mild GH optimization may improve how you feel in the short term, chronically pushing this axis harder is not clearly compatible with living much longer.
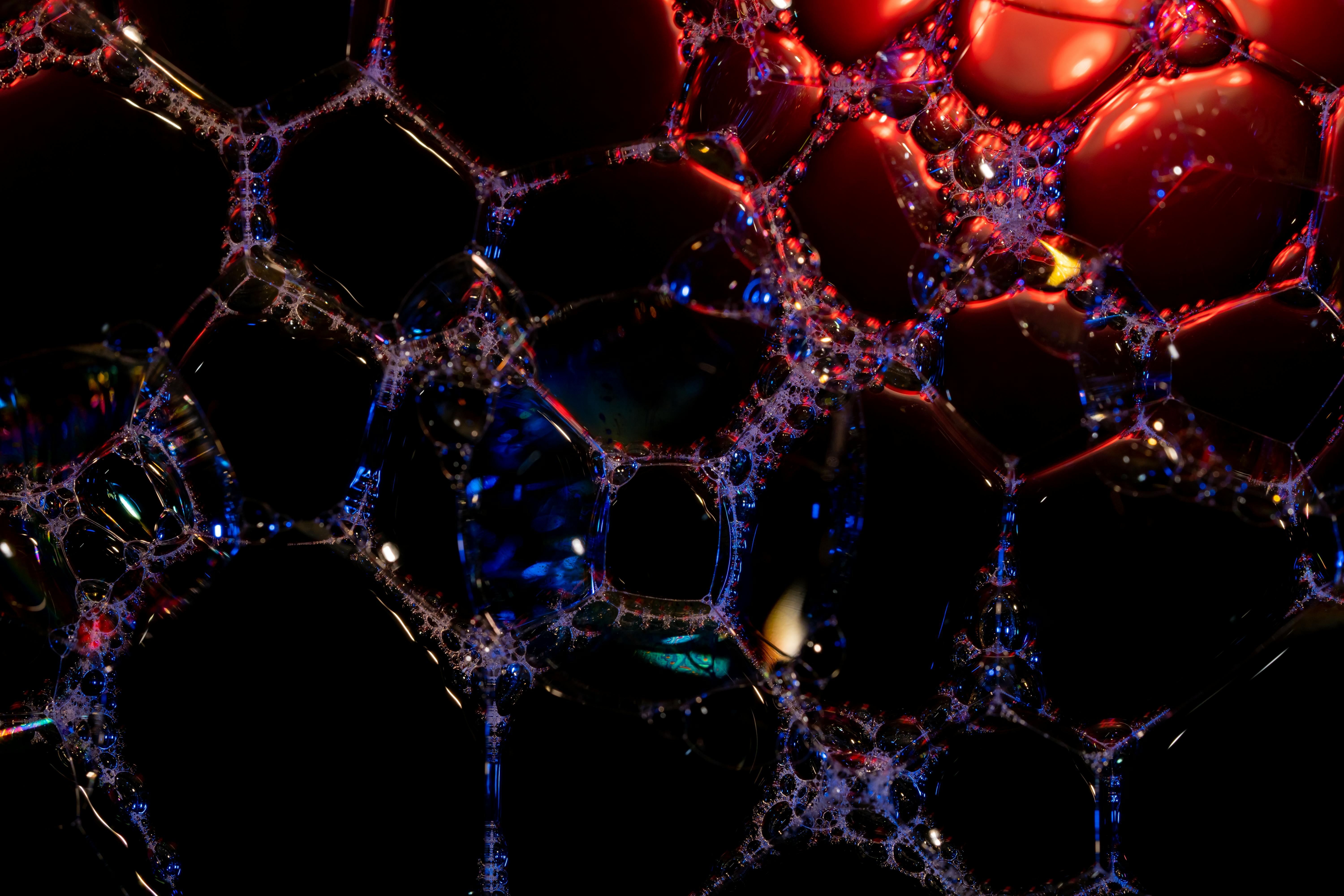
2. Tissue Repair and Regeneration Peptides
These peptides are marketed for “healing,” soft-tissue repair, and recovery:
- BPC‑157 – derived from a gastric protein, studied in animals for tendon, ligament, and gut healing
- TB‑500 – a synthetic fragment of thymosin beta‑4 involved in cell migration and angiogenesis
- Various “Wolverine stacks” combining BPC‑157 and TB‑500
Most of the excitement around these peptides comes from preclinical studies showing:
- Faster healing of tendon and ligament injuries in rodents
- Improved blood vessel formation around injured tissue
- Protection of gut mucosa in experimental models
But high-quality, randomized, long-term human data for these compounds are scarce. At the same time, the same mechanisms that stimulate repair—cell proliferation and new blood vessel growth—raise theoretical concerns about cancer risk or abnormal tissue growth over decades.[^topol]
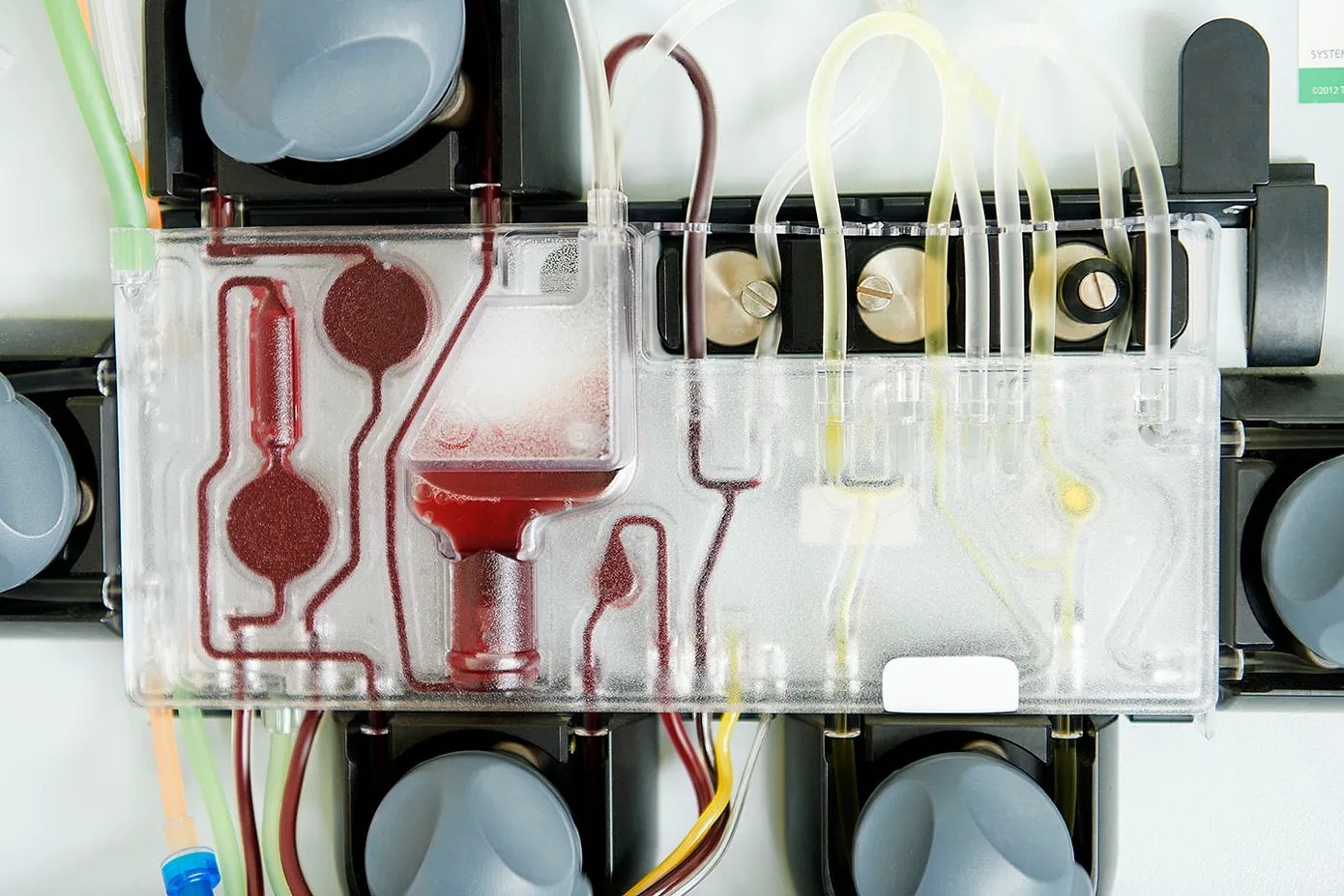
3. Metabolic and Body-Composition Peptides
This category includes:
- GLP‑1 receptor agonists (semaglutide, tirzepatide and related peptides)
- Tesamorelin for visceral fat in HIV-associated lipodystrophy
- Various experimental peptides that target fat oxidation or appetite
Here, the evidence is stronger—especially for GLP‑1 medications. Large randomized trials show:
- Significant weight loss
- Improvements in blood sugar and cardiovascular risk
- Potential benefits for fatty liver disease and heart failure
However, these drugs are not yet longevity interventions per se. They treat very real metabolic disease. Whether they extend lifespan in otherwise healthy, lean individuals is completely unknown.
4. Immune Modulating Peptides
Certain peptides, such as thymosin alpha‑1, LL‑37, and others, are studied for:
- Enhancing vaccine response
- Modulating immune activity in infections
- Potentially reshaping inflammatory pathways
In some countries, thymosin alpha‑1 is approved for specific immune indications, but its role as a generalized longevity peptide remains unproven. Many other immune-active peptides are still firmly in the experimental bucket.
The Evidence: What We Actually Know
When you pull back from marketing copy and look at the scientific literature, a consistent pattern emerges:
- There is robust evidence for a small number of peptide medications in defined diseases (GLP‑1s for diabetes and obesity, tesamorelin for HIV lipodystrophy, etc.).
- There is preclinical promise but limited human data for many of the most hyped “anti-aging” peptides (BPC‑157, TB‑500, Epitalon, GHK‑Cu, and growth hormone secretagogues combined for wellness).[^^atria][^topol]
- There are real safety and regulatory questions. The FDA has issued warning letters and flagged several peptide bulk substances—BPC‑157, LL‑37, thymosin beta‑4 fragments, injectable GHK‑Cu, CJC‑1295, and Ipamorelin—as potential safety concerns or unapproved drugs marketed inappropriately.[^atria]
In short: the science is interesting; the marketing is several steps ahead of the data.
How a Responsible Longevity Clinic Thinks About Peptides
From a clinician’s standpoint, peptides should be framed as tools, not magic bullets. A thoughtful peptide strategy typically involves:
-
Clarifying the primary objective
- Is the goal improved sleep, injury recovery, metabolic health, skin quality, or something else?
- Could this same outcome be achieved with simpler, better-studied interventions first?
-
Assessing baseline risk
- History of cancer or precancerous lesions
- Uncontrolled autoimmune or inflammatory disease
- Severe metabolic dysfunction
-
Prioritizing foundational work before advanced tools
- Nutrition, movement, sleep, stress management, and environmental exposures still move the needle more than any peptide protocol.
-
Using regulatory context as a signal
- FDA-approved peptides with defined indications and human data belong in a different risk–benefit category than unapproved “research peptides” compounded in small labs.
-
Keeping time horizon in view
- Many peptides are studied over weeks or months. Longevity strategies must consider decades.
Where Peptides Might Fit in an Anti-Aging Strategy
Within a comprehensive, medically supervised longevity program, peptides may play focused, adjunctive roles:
1. Recovery and Rehabilitation
For highly active individuals, the appeal of faster soft-tissue healing is obvious. While hard human outcome data are limited, carefully selected repair-oriented peptides may be considered in:
- Post-surgical rehabilitation
- Recurrent soft-tissue injuries in athletes
- Chronic tendinopathies not responding to standard care
In these settings, the goal is not “anti-aging” in the abstract, but targeted function: getting someone out of pain and back to movement, which indirectly supports long-term healthspan.
2. Metabolic Reset in High-Risk Patients
In individuals with:
- Established type 2 diabetes
- Severe obesity
- Fatty liver disease
GLP‑1-based therapies can dramatically improve metabolic health, which is central to longevity. Here, the peptide is not a vanity tool—it is disease-modifying medicine.
3. Sleep, Body Composition, and Quality of Life
Growth hormone secretagogues are sometimes deployed to improve:
- Deep sleep and recovery
- Lean mass retention during weight loss
- Subjective vitality
Because of the unclear long-term implications of chronically elevated GH/IGF‑1, this approach requires nuanced risk–benefit discussions, conservative dosing, regular monitoring, and very careful patient selection.
Common Myths About Peptides and Anti-Aging
Myth 1: “Peptides are natural, so they’re automatically safe.”
Reality: Many “natural” signals in the body are tightly regulated for a reason. Turn them up too far or for too long, and problems appear. Growth hormone, inflammatory cytokines, and angiogenic factors are prime examples.
Myth 2: “If bodybuilders use it, it must work.”
Bodybuilders, biohackers, and longevity enthusiasts are often the earliest adopters of new compounds. Their n=1 anecdotes can generate useful hypotheses, but they are not substitutes for controlled trials—especially when the same individuals are stacking multiple drugs, supplements, and training modalities.
Myth 3: “If it’s offered at a clinic, it has been thoroughly vetted.”
The regulatory framework for wellness clinics is not the same as for pharmaceutical companies. The fact that a peptide is compounded and injected in a spa-like setting does not mean it has passed large, long-term, randomized trials.
Myth 4: “Peptides will replace the basics of longevity.”
No peptide protocol can outrun chronic sleep deprivation, visceral obesity, continuous ultra-processed food intake, or untreated hypertension. At best, peptides are a layer on top of the fundamentals.
Building a Peptide Roadmap That Makes Sense
If you are considering peptide therapy as part of an anti-aging plan, it can be helpful to follow a staged decision process with your clinician.
Stage 1: Foundations and Diagnostics
- Comprehensive lab work: metabolic, hormonal, inflammatory, and nutrient markers
- Body composition analysis and visceral fat assessment
- Sleep and circadian rhythm profiling
- Evaluation of musculoskeletal limitations and injury history
The output of this stage is a clear map of your true leverage points. Sometimes the best intervention turns out to be strength training, time-restricted eating, or addressing sleep apnea—not a peptide vial.
Stage 2: Targeted Use Cases
Only after foundations are in place does it make sense to ask where peptides might add incremental value. Examples:
- A GLP‑1 analog for a high-risk patient with severe insulin resistance, combined with nutrition and resistance training.
- A short, time-limited course of tissue-repair peptides around a major orthopedic surgery, as part of a broader rehab plan.
- Carefully monitored growth hormone secretagogues in a narrow set of cases where low GH is clearly impairing quality of life, and other strategies have been exhausted.
Stage 3: Ongoing Monitoring and Course Correction
Any peptide protocol worthy of being called “longevity medicine” should include:
- Regular lab monitoring and imaging where appropriate
- Objective tracking of sleep, strength, body composition, and function
- Clear stop conditions if risks outweigh benefits
The Bottom Line on Peptides and Longevity
Peptide therapy is one of the most exciting and confusing areas in modern anti-aging medicine. On one hand, we have:
- Decades of basic science showing that short amino acid chains can precisely modulate cellular pathways.
- Legitimate, approved peptide drugs transforming the treatment of metabolic disease and other conditions.
On the other hand:
- Many popular “longevity” peptides lack robust human data on healthspan or lifespan.
- Regulatory oversight is patchy, and some compounds have been explicitly flagged as safety concerns by the FDA.[^atria]
- The same growth and repair pathways peptides target could, if overstimulated, theoretically accelerate certain age-related diseases rather than prevent them.[^topol]
Peptides are best viewed as specialized instruments in a much larger longevity toolkit—tools that should be used thoughtfully, sparingly, and with full awareness of how much we still do not know.
The most powerful anti-aging “stack” remains surprisingly low-tech:
- Metabolic health
- Strength and muscle mass
- Deep, regular sleep
- Emotional resilience and social connection
Peptides may help some people layer additional benefits on top of these fundamentals—but they cannot replace them.